Research is coming internationally on the long term effects of COVID-19. There has been an appalling trend for thousands of COVID survivors to remain debilitated by severe fatigue, brain fog, and tachycardia with a resulting inability to return to work. The economic implications of this with huge numbers of the 20 to 40 year old’s unable to work is hard to ignore, this accounts for 10-30% of those affected by the virus.
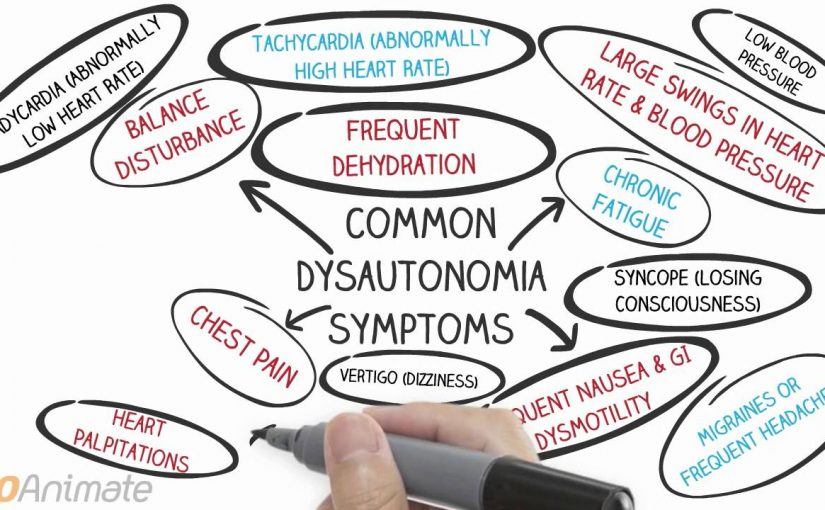
Amazingly some headway is being made into how to rehabilitate these patients. Unfortunately it is not a quick fix with a pill or a vaccination. The team at Mount Sinai Centre for Post COVID Care have found these people have developed ‘Dysautonomia’ or a dysregulation of the autonomic nervous system. Meaning their body is out of balance and struggling to cope with the smallest everyday actions, a bit like chronic fatigue syndrome or an immune disease.
This lack of balance is impacting on heart rhythm, blood pressure, temperature, fight and flight responses and a myriad of other functions such as digestion, cognition and breathing.
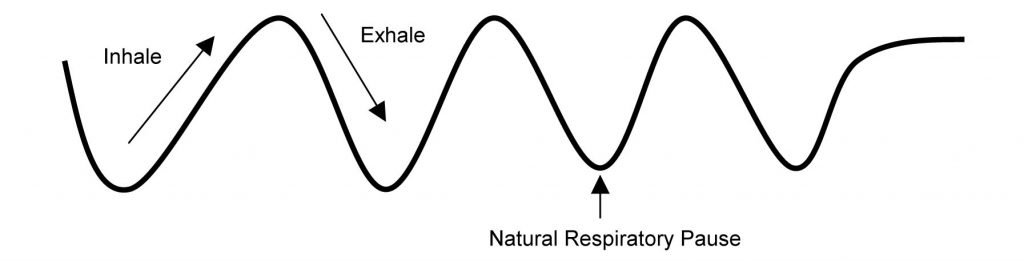
So how have they been making a positive change in these people’s lives? Well apart from dietary changes, stress management and individual rehabilitation programs they introduced a new breath management system called ‘Stasis’ which helps to regulate the body with interval breathing practice morning and night. This works to coach the body back into a regular rhythm and start to restore balance needed for them to get mobilising again without shallow breathing and spiking heart rate leaving them bedridden.
Good news for those who are struggling after contracting COVID-19 to get back to work and their daily routines. At least they can put a name to it and know that they are not malingering and seek help from a breath management service.