I have recently been working with a patient who describes herself as a person who likes to just get in and get the job done. We have had a bit of a journey to find a tool that helps her to slow her rate and gain control not just physically but mentally when she gets breathless following exertion.
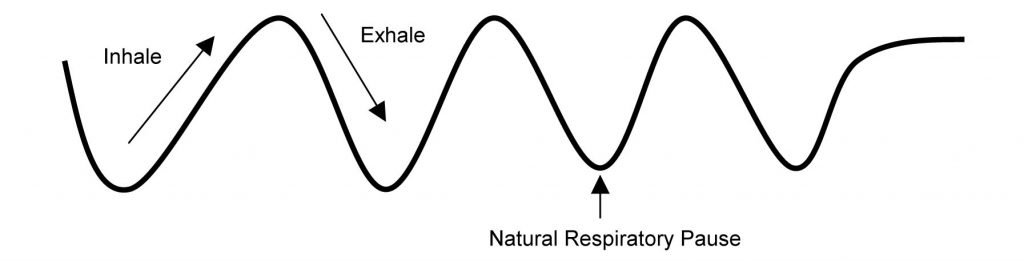
I have been using patterns of breathing, with oxygen saturation and heart rate monitoring, to influence the recovery rate of the individual during and post activity. There is much in the literature about resonance breathing to help you relax faster when stressed using the natural respiratory pause at the end of the extended exhalation. Shooting and marksman sports use this natural pause to steady themselves.
Adding a visual cue to this patterning such as used in the breath in a box technique can give a focus mentally and a rhythm to follow that can help slow the rate and help the person relax more easily. Everyone’s condition is different so it is important to find the rhythm that is comfortable for you and improves your self management in the moment of breathlessness. Daily practice will help you to improve.