Memories are special. The ones you want to hold onto need to be filled with detail to lessen the chance of losing it.
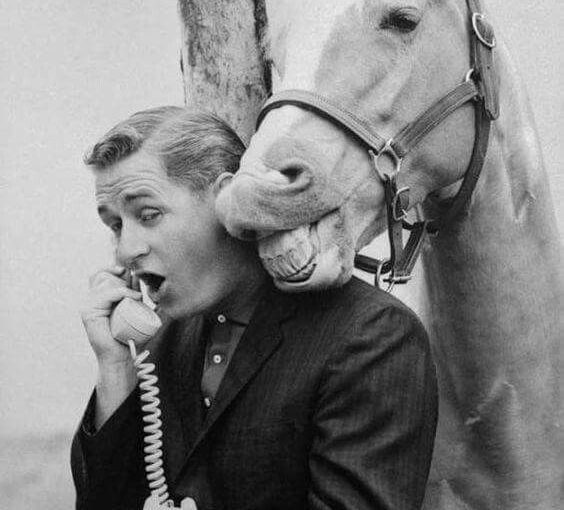
A good memory I have of one of my patients, and friend, is of an elderly gent sitting at his dining room table in a blue checked flannel shirt tightly tucked in, oxygen tubing stretched across his pale creased face, his side burns extra short from a recent “lowering of the ears” ,the skin on these patches almost white. The hair combed back and still wet from grooming himself that morning. His face intently focused on the pen in his hand making sketching’s in his pad of a horse in mid flight racing round the bend at a high stakes meet, all the while talking about his week, the incidences of daily life, the difficulties, the appointments, and then he pauses and looks up and with interest and intent in his eyes he says “And how are you?”
Always asking about other’s stories and lives giving pearls of wisdom in the form of his own experiences, he had a focus on optimising his self improvement throughout the course of his chronic illness. He often shared and was deeply interested in the works of:
- Emiold Coue a French psychologist known for auto suggestion – every day in every way I’m getting better was the mantra he found helped him.
- Maxwell Maltz who was an American cosmetic surgeon and author of Psycho-Cybernetics (1960), which was a system of ideas using self talk that he claimed could improve one’s self-image leading to a more successful and fulfilling life.
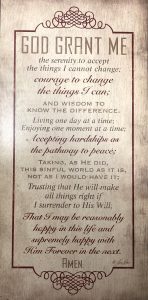
- and lastly the Serenity Prayer, a source of inspiration that often helped him get through the roller coaster of ill health.
My memory of conversations about his work as a Posty, his interest in bands and the great musicians of his time ….., his drawing and painting of iconic characters, military scenes and horses, a recent interest in one line portraits, all the while scribbling in his drawing pad as we talked, shaping and forming pictures from his minds eye whilst he thought on the issues that mattered most to him; grieving the loss of old friends , and caring for his wife, family and friends. He will be sorely missed.